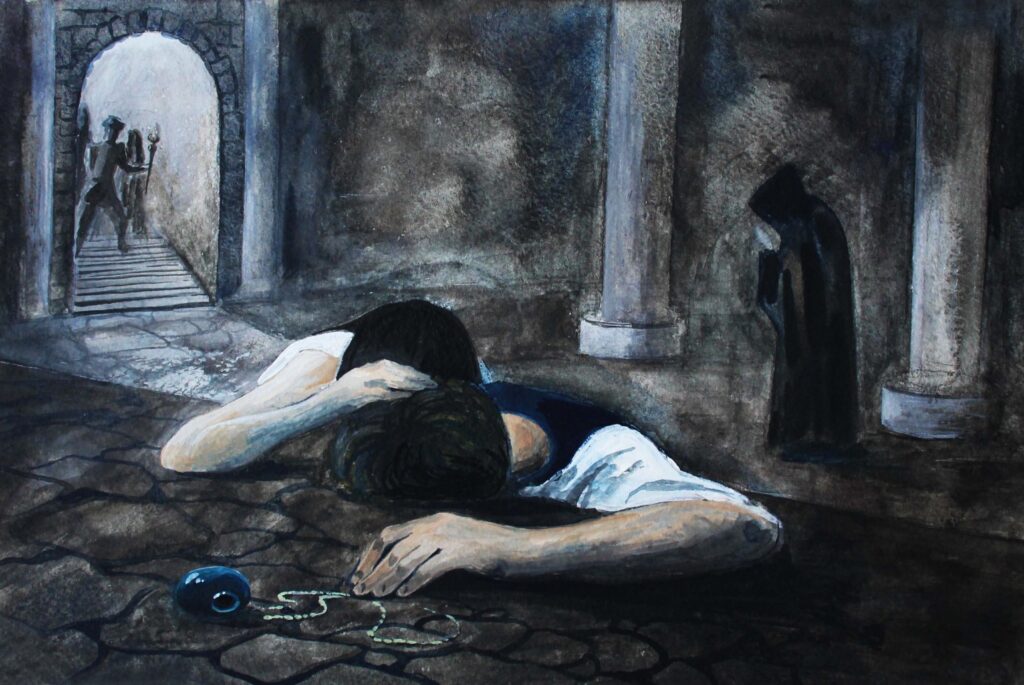
If you are going through hell, keep going
Winston Churchill
By the time patients come to me for the treatment of their depression, they have often been sick for some time. When we go into the history of the illness, it becomes clear that most have been depressed before. If you have had two episodes, more than likely, you will have a third one. If you have had three episodes, there’s a 90 percent chance you will have a 4th. Sadly, it seems that a single episode of depression is more the exception than the rule.
It is not hopeless. You can feel healed again.
If you find a medication or medication combination that works, stick with it. There is a huge temptation to to stop medication once you are feeling better. Even the most compliant of patients tend to stop medication around the 100 day mark. We now know that stopping meds is a huge trigger for relapse. The current recommendation is that you have to continue with medication for at least 2 years before thinking about stopping, and certainly not without your psychiatrist’s blessing.
Nowadays there are options if there is partial response or bad side effects. There are other treatment modalities available like TMS (transcranial magnetic stimulation). TMS has been proven as a very effective augmentation strategy in the treatment of depression. TMS is now available in Cape Town.
The current thinking is to treat depression, and to treat it hard. That includes tackling related conditions like addiction, anxiety and insomnia.
I always tell my patients that getting ill with depression is a huge stop sign. You have to stop and assess what is needed to prioritise your mental health. The aim is to get well and stay well.
- Your relationship with your psychiatrist
Treating depression is a rough road. Often the meds are not exactly right; often they are plain wrong. Sometimes patients have suffered in silence for so long that they don’t know how to speak for themselves. Helplessness and hopelessness are symptoms of depression. You need a psychiatrist who is accessible and whom you trust.
- Your relationship with your body
I always feel like such a Nazi when someone tells me how hard it was to get out of bed and I respond by telling them that they must move every day; to start off with some walking and build up to actual exercise. As glib as it sounds, there is a lot of evidence for the benefits of exercise in the management of depression.
When you are depressed, with no energy, there is either appetite loss or craving for carbs and sugars. Sugar briefly gives energy; carbs can briefly make us feel a little less empty. Unfortunately, too much is pro-inflammatory. Depression can be an inflammatory illness, so the last thing you need is a diet which makes things worse.
It is useful to think about supplements. Your brain needs building blocks to assist it with recovery. This is in addition to the antidepressants, not instead of.
- Omega 3 fatty acids: as found in deep water fish. A sushi habit can be expensive, but in tablet form 1000mg-2000mg of omega 3’s per day not only helps in depression, it is also anti-inflammatory and beneficial to the cardiovascular system.
- Folic acid (Vit B9) is the new blockbuster of antidepressant vitamins. It is needed in the brain for lots of essential things like enzyme actions and cellular metabolism. Found in grains, fruits, vegetables and beans, folate needs to be absorbed from the gut and then passes into the brain in the l-methyl-folate version. The problem is that genetics and many medications (even contraceptives) can stop this from happening. So even with a good diet people can be short of folate in their brain. The solution to this is to take high doses (more than 15mg) of folic acid or buy the slightly more expensive l-methyl-folate vitamin preparations.
- The super 4 of brain functioning: Calcium, Magnesium, Zinc and vitamin B12.
The is much research about the benefits of the supplements NAC and SAMe, but now it can start getting very expensive, so I usually only recommend these in specific cases.
Getting diet and exercise right is hard when you feel that getting out of bed is a challenge. It’s devastating how depression separates one from basic rhythms of sleeping when tired, getting up when rested, eating when hungry. I always encourage my patients to start a daily structure around eating times, sleep times, exercise and reflection. With a structure, my depressed patients don’t need to think. They just need to the next thing. As health improves this basic structure gets widened to include family, work and social times. Keeping to a structure where mental health is prioritised is essential and must continue in order to help to build resilience.
- Relationship with others
The risk for relapse is much higher if toxic relationships continue. When I work with someone who is depressed, I do not encourage them to leave relationships while they are sick (unless there is abuse, of course). I have learnt how the depressed brain can interpret everything in a paranoid or cynical way, and how this can impair judgement. If they complain bitterly about a relationship, I encourage them to get strong first, then review the situation. But what I do start working on, right from the beginning, is boundaries. It is a skill which many of us are lacking and can add to us feeling helpless in many situations. The basic premise of boundaries is not to take on other people’s issues and to hold steady in not letting them take on yours. Psychotherapy is the class room to help figure out your
- Relationship with work
Depression has a terrible symptom of impairing memory and concentration and increasing anxiety and feelings that they are not performing in the sufferer. Negative cycles are set up: the boss gives them a hard time, which affirms this view. Many of my patients come to me not only depressed but utterly depleted from working 16 hour days in an endless attempt to catch up. Again, I discourage people from resigning while they are ill. Getting back to work is an important part of recovery. I do encourage them to take time off to give recovery space to happen. And, when they are well, to plan regular holidays to stay well.
- Relationship with one’s spirituality
For me, spirituality is that sense of connection with the universe and one’s place amongst all living things. There has been much research validating the healing power of prayer and the benefits of mindfulness.
For some people, connecting with their spirituality would be reconnecting with their religion. For others, it’s meditation and others yet find benefits in journalling. Whatever works for you, it involves consciously putting quiet time aside to be with oneself. Today’s world of constant stimulation makes us feel frazzled and disconnected.
One of my patients told me that her life had been very hard, tormented by repeated breakdowns. But all the work that she has had to do to prioritise her mental health has meant that it has become very rich. Not everybody works that hard to get well and stay well. It is worth remembering that while the idea of a single episode of depression seems wishful, this horrible illness does not need to define you.






